For GPs and Other Health Professionals


The incidence of cancer is rising in Australia and co-ordination of care between health professionals is essential. This section is aimed at providing information on radiation therapy (also called radiotherapy) for any health professional involved in a patient’s cancer care with a particular focus on primary care providers.
GP Oncology Education Evenings
Useful resources for GPs
-
-
The importance of General Practitioner (GP) involvement
GPs play a crucial role at every stage in the management of a patient diagnosed with cancer.
The trusting relationship that exists between a patient and their GP optimises the delivery of health care – from the time of initial diagnosis to treatment planning, surveillance and transition to survivorship or palliative care.
As a general practitioner, your role may include some or all of the following:
- Initial investigations and diagnosis
- Informing the patient and their family of the diagnosis
- Referral to a Radiation Oncologist for an opinion at diagnosis (see indications below)
- Referral to and liaison with other specialists
- Assisting with treatment decisions
- Providing psychological support
- Optimising co-morbidities
- Continuation of preventative care
- On-going monitoring/follow-up
- Recognition and management of cancer-related symptoms
- Referral of patients for radiation therapy for palliation of symptoms such as bone pain (see below Is radiation therapy indicated for my patient? )
- Recognition of, and referral for, management of cancer-related emergencies
- Recognition and management of acute side effects and rarer long-term complications of cancer therapies
- End of life care
- Assisting with the many issues arising for families and carers.
-
Is radiation therapy indicated for my patient?
Radiation therapy can be utilised across a variety of indications in the treatment of almost all cancers. Depending on the clinical scenario, radiation therapy may have an important role as a:
- Definitive treatment (primary/radical)
- Adjuvant treatment (post-operatively)
- Neo-adjuvant treatment (pre-operatively)
- Combined treatment with chemotherapy (chemoradiation) and/or
- Palliative treatment
For further information click on the icons below to view relevant tables and graphs:
Table 1: Is radiation therapy indicated for my patient?
Click To View Table 1 – Is radiation therapy indicated for my patient?
Graph 1: Ideal utilisation of radiation therapy (RT) for common tumours types i.e. percentage of patients for that cancer benefiting from RT based on best available evidence4
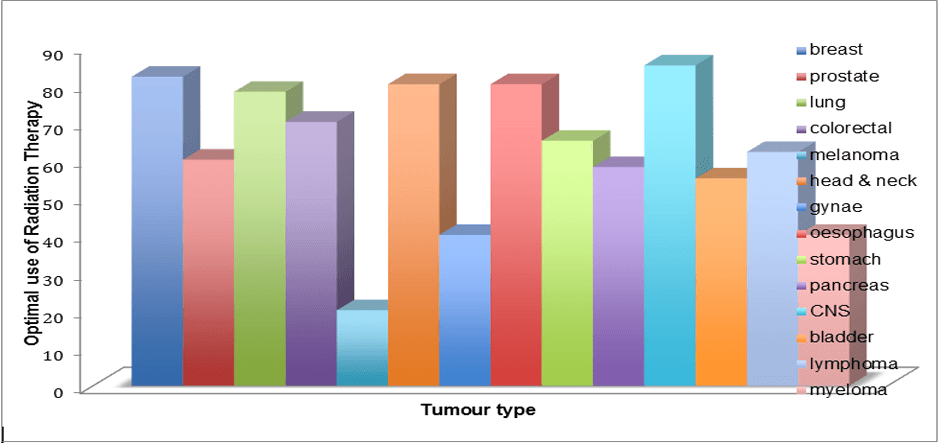
Unfortunately not all patients who might benefit from radiation therapy receive it.
There are several reasons for this, including the lack of access for some patients and lack of awareness amongst some health professionals.
Graph 1 above shows the proportion of patients who would benefit from having radiation therapy as part of their cancer treatment, according to tumour type.
These numbers are based on the best available evidence in the literature.
-
Patients with a known history of cancer, even if not diagnosed with metastases, need to be referred urgently if they have any symptoms or signs of possible malignant spinal cord compression (MSCC).
Giving radiation therapy (with or without an operation) is the most important predictor of a person remaining ambulant after having cord compression. Unfortunately delay in diagnosis is common and this will result in permanent paraparesis.
Signs of MSCC are shown in the table of cancer related emergencies along with other clinical situations where prompt referral for radiation therapy is important.
Cancer patients with pain should also be sent promptly for assessment by a Radiation Oncologist, Palliative Care Physician and/or other cancer specialist.
Radiation therapy is a simple and effective way to alleviate pain caused by cancer involving the bones. Short courses of radiation therapy (even a single treatment) have around an 80% chance of reducing, or even eliminating pain altogether (also see About radiation therapy – what is radiation therapy used for?).
Table 2: Cancer related emergencies
Click To View Table 2 – Cancer related emergencies
-
How do I refer to a Radiation Oncologist?
The referral pathway for a patient will vary according to each individual situation. Patients can be referred to a Radiation Oncologist by one or more of the following methods:
- Direct GP referral
- Specialist referral (Surgeon, Medical Oncologist, Haematologist, Gynaecological Oncologist, Paediatric Oncologist, Dermatologist, Palliative Care Physician etc.)
- During an inpatient admission
- At a multidisciplinary cancer care team meeting.
Patients are often seen in the first instance by a Surgeon or Medical Oncologist. They may not always be referred to a Radiation Oncologist by these specialists, even in circumstances where radiation therapy offers an equivalent curative treatment option, such as for localised prostate cancer.
It is important that as a GP, both you and your patient are informed about the potential role of radiation therapy in your patient’s cancer care management. Referring your patient to a Radiation Oncologist may assist your patient and their family in making an informed decision about their cancer treatment by enabling them to fully explore all therapeutic options.
A list of Radiation Oncologists and radiation oncology treatment centres can be accessed through our Treatment Centres page.
-
Understanding your patient’s radiation therapy
Details of the Radiation Oncologist’s plan of management will be summarised in the initial consultation letter.
This should outline your patient’s diagnosis and current symptoms as well as the site and aims of their treatment. It should also indicate whether other treatment options are available and the risk to benefit ratio of radiation therapy. Written communication will document the other specialists involved in your patient’s care and the proposed follow-up plan.
A treatment summary will be sent to you at the completion of your patient’s radiation therapy. This letter will likely include some technical details of treatment such as the dose and number of treatments or fractions. It will also document any acute side effects experienced, the severity of these and how they might be managed.
The information below will assist you in understanding some of the technical parameters used in the delivery and description of radiation therapy.
Understanding treatment summaries:
Treatment intent
- Either definitive, adjuvant, neoadjuvant or palliative (see Is radiation therapy indicated for my patient?)
Radiation dose
- This is reported in Gray (Gy). 1 Gy is the absorption of one joule of energy, in the form of ionising radiation, divided by one kilogram of matter.
- The dose chosen by the Radiation Oncologist will depend on many things including the intent of treatment, tumour pathological features and patient factors. Curative schedules are typically in the range of 40 to 70Gy while palliative schedules are lower with doses of 8-30Gy.
Number of fractions
- A fraction refers to the number of treatments that are delivered e.g. 20 Gy in 5 fractions indicates that 5 treatments of 4 Gy each where delivered.
Side effects from treatment
- Side effects of treatment may be graded from 1-4 according to severity.
(Also see What are the side effects and FAQs)
-
Communicating with the Radiation Oncologist
Communication amongst health professionals is vital in delivering optimal care for a patient. Please feel free to call the Radiation Oncologist involved in your patient’s care if you have any questions or concerns relating to their treatment. Copies of all letters sent to other doctors should also be sent to you, but sometimes systems do not work as effectively as they should. Again, do not hesitate to call the Radiation Oncologist or registrar involved with your patient’s care. Similarly, the treating team may call you to clarify certain aspects of your patient’s management.
Some things which may be useful to discuss might include:
- Your patient’s current management plan
- The suitability of a referral for a radiation oncology opinion
- Making an urgent referral
- Side effects of treatment
- Admission to hospital and/or transfer of care
- Providing end-of-life care.
-
Follow-up care
With increasing numbers of cancer survivors, GPs or other primary health care providers play an important role in follow-up care. Acute side effects from your patient’s radiation therapy will usually be temporary and are managed within the follow up care provided by the Radiation Oncologist. These side effects may occur during treatment or just after its completion and usually resolve within six to eight weeks.3
A small percentage of patients may experience late side effects from radiation therapy and in most cases they will present in the first instance to their GP.3 Late adverse effects may be noted months to years after treatment.3 Although rare, secondary malignancies from radiation therapy may manifest 10 to 30 years after a patient’s initial treatment. The risk of a secondary malignancy is higher for certain types of radiation treatments and is considerably higher for patients treated as children or young adults. (Click here for further information)
-
Managing side effects
Most of the acute side effects experienced by a patient will resolve within 8 weeks of completing treatment. Managing these during and after the treatment is important to optimise patient adherence to treatment and to minimise the impact of radiation therapy on a patient’s quality of life. Most of these side effects will be addressed by the Radiation Oncologist during treatment and follow up.
Find more information about side effects
-
Caring for special populations having radiation therapy
Paediatric patients
Children with cancer will be managed in comprehensive paediatric cancer teams involving Radiation Oncologists, Medical Oncologists, Surgeons and other multidisciplinary health care professionals. The team will work together with the GP to address the complex medical and psychological issues faced by children and their families.
Adolescents and Young Adult (AYA) patients
AYA patients may present with tumour types that are commonly seen in either paediatric or adult patients. Additionally, AYA patients have specific medical, psychological and social issues that need to be managed during their treatment such as consideration of fertility preservation and educational and/or vocational support. Specialist teams have been developed to address the unique needs of AYA patients who have been diagnosed with cancer. Some useful links are listed below.
- Referral information for AYA teams can be found on Canrefer
- All AYA patients with sarcoma should be referred to a specialist sarcoma centre for treatment where the Surgeon, Radiation Oncologist and Medical Oncologist will work together closely. For details of centres that specialise in sarcoma care, visit the Australasian Sarcoma Study Group.
- Additional support information can be accessed through CanTeen Australia, CanTeen New Zealand and Child Care Foundation New Zealand.
Adult survivors of childhood cancer
Most adult survivors of childhood cancer receive their medical care from their general practitioners. The chronic issues faced by these patients may be unfamiliar to community practitioners. However, it is important to ensure that if required, appropriate follow-up and long-term care is carried out.
Guidelines have been developed to assist with long-term follow-up care. These will enable you to understand a survivor’s risk, provide additional screening as needed and to identify late adverse effects of childhood cancers.
In addition to providing medical care, GPs of childhood cancer survivors need to perform surveillance for secondary cancers, identify late effects of therapy and attend to psychosocial needs. Plans should be individualised and based on the patient’s risks of various late adverse effects. (See reference 6 for further information)
-
Rural and remote perspective
The referral base for many of the radiation oncology departments in Australia and New Zealand extends across rural and remote regions. This necessitates rural patients who require radiation therapy to relocate to an area closer to the nearest radiation oncology department for the duration of their treatment. This may only be a single or weeklong treatment however in some cases, treatment courses can last up to 8 weeks. This relocation can have a significant financial and psychosocial impact on both the patient and their families. The GP also has a role in making sure the patient can access the closest treatment centre. In recent years many centres have been established in regional areas so that patients do not have to travel to the major cities.
Medistays enables patients, carers and healthcare professionals to find and book accommodation close to hospitals and medical facilities.
Following the completion of their treatment, rural patients return to their homes. Any acute side effects from radiation therapy may not have resolved on completion of their treatment.
In some instances, side effects may even increase in severity before beginning to resolve 10 to 14 days after treatment.
As a GP in a rural or remote region, you may be required to provide this acute care.
Please see managing side effects for further information to assist you in this.
-
References and further information
- Primary Care of the Patient with Cancer. Smith, George F and Toonen, Timothy R. 8, April 15, 2007, American Family Physician, Vol. 75, pp. 1207-1214.
- When to Consider Radiation Therapy for Your Patient. Tisdale, Bernard. 5, March 1, 1999, American Family Physician , Vol. 59, pp. 1177-1184.
- Managing the Adverse Effects of Radiation Therapy. Berkley, Franklin J. 4, August 15, 2010, American Family Physician , Vol. 82, pp. 381-388.
- The Role of Radiotherapy in Cancer Treatment. Delaney, Geoff, et al., et al. 6, September 15, 2005, Cancer, Vol. 104, pp. 1129-1137.
- The Role of General Practice in Cancer Care. Mitchell, Geoffrey. 9, 2008, Australian Family Physician, Vol. 37.
- Primary Care of Adult Survivors of Childhood Cancer. Seehusen, Dean A, Baird, Drew and Bode, David. 10, May 15, 2010, American Family Physician, Vol. 81, pp. 1250-1255.
Page last updated: 20/10/20