Particle Therapy

What is Particle Therapy?
Particle therapy is a specialised form of radiation therapy that may have benefits over conventional radiation therapy for some patients and conditions. Particle therapy is a form of external beam radiation therapy which uses beams of radiation with heavy particles and includes treatments such as proton and carbon ion therapy.
Particle therapy is most effective for treating tumours that are near important structures, such as the brain or spine, and have not spread elsewhere in the body. It may be more beneficial for young patients as it reduces the risk of harming healthy, growing tissue and minimises long-term side effects that may result from radiation therapy.
Conventional radiation therapy using x-rays (photons) or electrons, starts to deliver some of the radiation dose when it enters the body and continues to deliver a small amount of radiation dose after it has passed through the tumour. Increasingly, improvements in radiation therapy technology have enabled the radiation dose to healthy tissue to be kept to a minimum.
Particle therapy uses highly charged particles which deliver a smaller amount of radiation on their way to the tumour, delivering most of it to the tumour before stopping almost completely. This is known as the Bragg Peak. As a result, surrounding healthy tissue absorbs very little radiation and potentially there is a reduction in long term side effects.
-
-
Forms of Particle Therapy
Proton Therapy
The most common form of particle therapy is proton therapy, in which the beams of radiation are made up of protons. There are treating facilities in Europe, the USA and Asia.
Below is an example of a treatment room in a proton therapy facility. In the centre, there is a treatment bed or ‘couch’ (where the patient lies for treatment), and a rotating gantry (which holds the treatment head or ’nozzle’ – where the radiation beam exits the machine).

This is an example of a treatment room with a treatment bed or ‘couch’ which is held by a robotic arm.

This is an example of a cyclotron, one of several technologies that generate proton beams used for the treatment of cancer. It is housed underground away from patients and health care providers.|

This is an example of a synchrotron, another type of a technology used to deliver proton therapy for the treatment of cancer. It is also housed underground and away from patients and health care providers.
Carbon ion therapy
Carbon ion therapy is another type of particle therapy that is less commonly available, with only thirteen treatment centres in the world. Carbon ion therapy requires larger and more expensive equipment.
Carbon ions deliver more energy to the tumour and less to nearby normal tissues than proton therapy. Carbon ion therapy is beneficial for patients with tumours that are resistant to conventional forms of radiation therapy and proton therapy. It is not a treatment used for children who typically have tumours that respond well to conventional radiation and proton therapy.
-
How can I access particle therapy treatment?
Particle therapy is not yet available in Australia or New Zealand. The Australian Government provides financial assistance for Australian citizens or residents to receive medical treatment overseas when effective treatment is not available in Australia via the Medical Treatment Overseas Program (MTOP). Presently patients can access particle therapy treatment through this scheme. A similar scheme, called the High-Cost Treatment Pool may provide funding for New Zealand citizens.
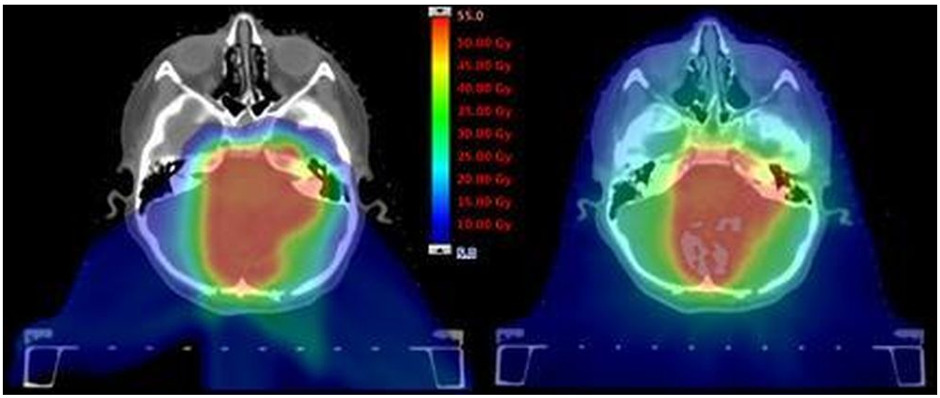
Currently an application for financial support through MTOP must include from the patient’s treating medical team, supporting information and evidence to show the benefits of treating the patient with particle therapy rather than conventional radiation therapy. Information needs to include a comparative radiation plan (a conventional plan and a proton plan) which the patient’s treating medical team organises. An example of comparative plan is provided below in Figure 1 with a proton therapy plan on the left and a conventional photon plan on the right. The red shaded areas demonstrate high dose to the tumour and the blue shaded areas show low dose to areas of the brain and other structures away from the tumour.
In recognition of the comparative advantages of proton therapy for some patients, the Federal Government announced funding in 2017 to purchase proton therapy equipment to treat patients in Australia. Commencement of the building to house Australia’s first proton therapy unit has begun, and will be housed in the Adelaide BioMed city.
More information about this project is available at Australian Bragg Centre. It is expected the Centre will be opened to treat the first patients in 2025.
Business cases have advanced for more than one treatment centre in Australia. There is a commitment from professional groups with expertise in radiation therapy and cancer care to ensure patients are selected for treatment according to agreed clinical need, and all facilities are working together to develop national protocols with consistent access to treatment. Clinical trials and other research in radiation oncology will be expanded to involve these new technologies and treatments will be conducted across Australia collaboratively to ensure high-quality patient care continues to be accessible to all who may benefit.
Who will be treated at the Australian Bragg centre?
The governance and decisions around who will receive funding for particle therapy once it is available in Australia are under development. Children, teenagers and young adults are expected to be a high priority.
-
What is involved in proton therapy treatment?
The treatment planning process for particle therapy is similar to conventional radiation therapy and requires the patient to have a Computed Tomography (CT) scan and sometimes a Magnetic Resonance Imaging (MRI) scan. This is performed in the treatment position (most often with the patient lying down on their back) and provides images of the tumour and the organs nearby to help the radiation therapy team (radiation oncologist, radiation therapist and medical physicist) make sure the best treatment plan is designed for the individual patient. Click here to learn more about the Radiation Oncology Team.
Like conventional radiation therapy, the patient won’t feel or see anything while the treatment is delivered each day. As the proton treatment is very precise and targeted it is important that the patient is comfortable and lies very still. Sometimes patients need to be fitted with an immobilisation shell or other equipment to help keep them in the correct position and immobile. Time in the treatment room can be longer for proton therapy each day (30 – 45 minutes) than conventional photon therapy (15 – 30 minutes) because of the more complex nature of the proton beam. Young children may require sedation each session to keep them still for treatment.
The side effects of proton therapy, while less than conventional radiation therapy, depend on the part of the body being treated, the size of the tumour and the types of healthy tissue near the tumour. It is important that you talk to your radiation therapy team about your treatment and any side effects you experience. They will be able to discuss the therapy process and give you information that is specific to your treatment.
-
Resources for understanding particle therapy
The short video below is an excellent explanation which will help you understand how particle therapy works: called ‘Curing Cancer with Proton Beams – Dr Suzie Sheehy.’ Dr Sheehy is a medical accelerator physicist at the University of Melbourne. In the video, she explains how radiation therapy works, what protons are and why they are useful in the treatment of certain cancers.
This video comes from the National Proton Therapy Centre at the Christie in the UK. It talks about access to proton therapy in the UK and the benefits that particle therapy provides for some patients.
A group of Australian physicists and doctors travelled to Japan to learn more about particle therapy technology as particle therapy has been used to treat patients in Japan and other countries for over 20 years. Go behind the scenes of the incredible facilities and see the technology that has treated tens-of-thousands of patients.
Get to know proton beam therapy from Australia’s Science Channel.
-
Frequently Asked Questions (FAQs)
-
-
Why aren’t all cancers treated with particle therapy instead of conventional radiation therapy?
Some patients will ask, “Why don’t we just use proton therapy all the time?” The answer is that modern conventional radiation therapy is very good at treating the majority of cancers whilst proton therapy is best for patients where the tumour is very close to critical structures of the body such as the spinal cord, and where reducing the dose to healthy tissue in young patients is important for ongoing development.
The radiation oncologist along with other members of a multidisciplinary team comprised of surgeons, medical oncologists (specialist doctors who prescribe chemotherapy), and other health care professionals, will make a decision that is based on the best available clinical evidence for each individual patient.
-
Does particle therapy treatment hurt?
No, the therapy is non-invasive. However, depending on the part of the body that is being treated, some patients might experience short- and long-term side effects. This also applies to conventional radiation therapy.
-
Are the side effects the same for both types of radiation therapy?
Side effects from particle/proton therapy are typically minimal and may be less than conventional radiation therapy because surrounding healthy tissues and organs receive lower radiation doses. Every patient’s experience will be different as side effects often depend on the part of the body receiving treatment and the treatment dose. -
How long after treatment will I be able to see a difference in the tumour size?
This will depend on the type of tumour being treated. Your radiation oncologist is best placed to explain this, as well as develop a follow-up program for you. -
How soon after treatment can I go back to normal activity?
Many patients are able to continue with their routine activities throughout the treatment, including working, exercising and socialising. If there are specific things that you should avoid doing during your treatment, a member of your treating team will discuss this with you. It is important to note that all patients are different, and some may have more difficulty with treatment than others due to a number of factors. Your treating team will look after you closely during and after your treatment. -
Will I have to wear a mask on my face?
Some patients need to wear an immobilisation shell (mask) to hold their head and neck still for their treatment, typically when the tumour is in the brain or head and neck area. Talk to your treating team if you have concerns about needing a mask for your treatment as there are several things that can be done to make wearing a mask easier. -
Can I use cream on my skin during treatment? If so, what is the best kind to use?
There are several things you can do to make yourself more comfortable if you have a skin reaction during your treatment. Talk to your treating team and they can provide advice that is specific to your treatment. -
Will I lose my appetite?
Some patients will experience a change in their appetite or taste during treatment. Each treatment course and patient is different. Most patients experience different reactions. Talk to your treating team and they will be able to explain what to expect with your treatment and give advice to help manage appetite-related side effects. -
What is the treatment room like?
The treatment room is spacious and open. The bed that patients lie on to receive treatment is placed towards the middle of the room and is called a treatment couch. Sometimes the couch will move slowly while you are lying on it, to place you in the correct position for your treatment. Some machines have a treatment head that looks as though it is attached to the wall. It will move around to treat you from different angles while you lie still on a couch that does not move. The treatment rooms may be a little cool. Your treatment staff will organise a blanket if you need one. -
Is it loud during the treatment?
You might hear a buzzing sound when the treatment is being delivered, but it is not loud, but you can still listen to music. -
How long does each treatment take to complete?
Treatment with photons or protons usually takes 30- 45 minutes per treatment, depending on the complexity of the treatment. Treatment is given once each working day. The average number of treatments that makes up a treatment course is approximately 20. -
Is proton therapy the best form of radiation for my cancer?
For specific cases, proton therapy can provide some advantages over conventional radiation therapy. However not all patients will benefit from this type of treatment. Talk to your radiation oncologist about which treatment option is best for you. For many patients, conventional radiation treatment remains the best option. -
Can proton therapy be used with other forms of treatment?
Yes. Proton therapy can be used with other types of treatment such as chemotherapy, immunotherapy and surgery. A multidisciplinary team of different specialist doctors will develop a treatment program that is specifically designed for each patient. -
Why can’t I access particle/proton therapy in Australia or New Zealand?
Particle therapy is an expensive technology needing a building larger than for conventional radiation therapy. Australia has committed to building one facility in Adelaide and other states are planning to build more in the future. Importantly, Australians are currently able to access modern conventional radiation therapy in all capital cities, and increasingly in regional and rural areas of Australia.
The Ministry of Health in New Zealand established a Cancer Control Agency in 2019. Priorities of the Agency include investment in technology and treatment capacity for radiation oncology.
Patient Stories
Until last year patients in the UK also had to travel abroad to receive particle therapy treatment. Here are some of their stories.
-
Useful links
Visit the Medical Treatment Overseas Program (MTOP) website to access information on applications to receive financial assistance for particle therapy treatment overseas, as it is not yet available in Australia. It is important to talk to your radiation oncologist who will advise you whether particle therapy may be an appropriate option for you or your child. If your radiation oncologist believes it is appropriate, he/she will complete the application form with you.
To submit an application to MTOP your radiation oncologist will need to provide evidence that treatment with protons would be significantly better than conventional radiation therapy that is available in Australia. Details for accessing the comparative planning service can be found on the Royal Adelaide Radiation Oncology Department – Comparative Planning Service website. It is important all patients talk to their radiation oncologist to get the right information about accessing particle therapy overseas before it is available in Australia.
New Zealand citizens or permanent residents may be considered for treatment funded under the Ministry of Health’s High Cost Treatment Pool.
ANSTO – The Australian Nuclear Science and Technology Organisation is one of Australia’s largest public research organisations. ANSTO is one of the key stakeholders that will help to setup and support particle therapy treatment and research in Australia.
The South Australian Health and Medical Research Institute (SAHMRI) is leading the project which will be housed in the basement of the Australian Bragg Centre building. Construction is well underway, the design of the physical build being refined with a team of national and international architects, engineers, and radiation specialists. It will be located in the heart of the Adelaide CBD and next to the Royal Adelaide Hospital and existing SAHMRI building. The facility will be the first in Australia to provide this type of treatment and is due to be completed in 2025.
Click here to see details of the proposal for a particle therapy (Carbon Ion) facility at Westmead in Sydney.
National Particle Therapy Symposia – Four national Symposia have been held in Adelaide (November 2017), western Sydney (July 2018), Brisbane (March 2019) and Melbourne (December 2020). They have brought together the parties across Australia that have developed business cases for a particle therapy facility, as well as key stakeholders from universities and government organisations and consumers. Experts in the field of particle therapy from across Australia and New Zealand are being identified and brought together to bring particle therapy to Australia and New Zealand in a co-ordinated, collegiate and collaborative way. Read the communiqué from the 2020 Particle Therapy Symposium.
Royal Australian and New Zealand College of Radiologists (RANZCR) Particle Therapy position paper – This position paper was developed by the governing body for radiation oncology in Australia on Particle Therapy in 2015. It was updated in 2022.
A summary statement by the Faculty of Radiation Oncology supports patients in Australia and New Zealand having access to particle therapy. The position paper informs doctors, health professionals, patients and interested individuals about the current status of particle therapy internationally and the evidence for its use. It aims to help identify the tumour types and locations for which particle therapy is the most appropriate treatment. The statement outlines the endorsed process for assessing Australian and New Zealand patients for referral overseas for particle therapy.
The Australasian College of Physical Sciences and Engineers in Medicine (ACPSEM) and Australian Society of Medical Imaging and Radiation Therapy (ASMIRT) are also involved in bringing particle therapy to Australia. Members of these organisations will be responsible for providing the quality assurance for all aspects of particle therapy planning and treatment delivery as well as planning and delivering particle therapy.
Page last updated: 26/02/2021