Head and Neck Cancer

Head and neck cancers include a variety of cancers that arise in the head and neck region. There are four main areas where these cancers occur which are described and depicte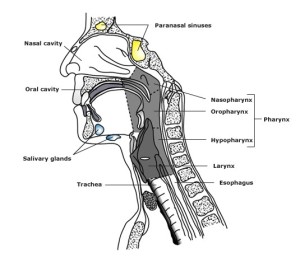 d in the next section.
d in the next section.
There are several cancers that can occur in this region but the most common type of cancer is squamous cell carcinoma (commonly referred to as SCC).
Most of the surfaces in the head and neck region are lined by mucosa. Cells within the mucosa can grow abnormally and at uncontrolled rates giving rise to SCC.
-
-
Location of Head and Neck Cancers
- Nasal cavity and sinuses: The nasal cavity refers to the nose and the structures within it. The sinuses are air-filled spaces within the bones of the face.
- Oral cavity: This area includes all the structures with the mouth, from the lips to the base of the tongue.
- Throat: This is an area that includes the pharynx and larynx. The pharynx is the area at the back of the nose, mouth and neck that is divided into three separate regions – the nasopharynx, oropharynx and hypopharynx. The nasopharynx is a passage behind the nasal cavity. The oropharynx lies behind the oral cavity. The hypopharynx refers to the lowest part of the pharynx. The larynx is the area that contains the vocal cords and other surrounding structures.
- Salivary glands: These glands are important in producing saliva that help to digest food. The main salivary glands are called the parotid glands, submandibular and sublingual glands.
Cancers can arise within any of the above sites and/or structures.
-
What are the Causes of Head and Neck Cancers?
The most common type of cancer seen in the head and neck region is squamous cell carcinoma (commonly referred to as SCC). Risk factors for developing a head and neck cancer include:
- Smoking: This is the most important risk factor. Smoking, especially with alcohol consumption, increases the chance of developing head and neck cancer.
- Alcohol consumption
- Genetic and ethnic differences
- Viruses such as the human papillomavirus (HPV): Cancers associated with this virus occur mainly within the tonsils and tongue base. These cancers behave differently to SCC and have different treatment outcomes. A test can be performed to determine if a cancer is HPV related.
- Betel- nut chewing
- Radiation exposure
- Vitamin deficiencies
-
What are the Symptoms of Head and Neck Cancers?
The symptoms of head and neck cancer will vary depending upon where the cancer is located. General symptoms may include:
- loss of appetite,
- weight loss and
A lump in the neck is a common symptom that can be associated with all types of head and neck cancers. The common symptoms for each specific area are listed below:
Nasal cavity or nasopharyngeal cancers: A common symptom is a lump in the neck. Other symptoms may be:
- nose bleeds,
- persistent blocked nose or
- changes to hearing which could be either hearing loss or a ringing sensation in the ears.
Pain may also be present at the back of the nose or in the ear.
Oral cavity or oropharynx cancers: Common symptoms include
- an ulcer of the lining of the mouth,
- tongue or lip that doesn’t heal,
- pain or difficulty on swallowing,
- bleeding from the lining of the mouth or gums,
- difficulty speaking or numbness of the chin.
Tumours in the oropharynx can result in snoring at night, bleeding from the mouth or a lump in the neck.
Hypopharynx cancers: Symptoms can include difficulty or pain with swallowing or a lump in the neck.
Larynx cancers: Common symptoms include:
- a hoarse voice,
- difficulty or pain on swallowing,
- chronic dry cough,
- pain in the ear,
- coughing up blood,
- difficulty breathing or shortness of breath and
- a lump in the neck.
Sinus cancers: These cancers may result in bleeding from the nose or a chronically blocked nose.
-
What are the Treatments for Head and Neck Cancer?
Head and neck cancers vary a lot in terms of where they arise as well as the specific type. Treatment for head and neck cancers will depend upon the location and type of cancer as well as the person’s individual features and risk factors. Broadly speaking, curative treatment options are radiation therapy and surgery. In some situations, chemotherapy may be given in combination with radiation therapy.
The type and sequence of treatment recommended for a particular patient will be decided by a team of different specialist doctors and other health professionals, often referred to as the Multidisciplinary Team.
The team involved in your care includes radiation oncologists, surgeons (ear, nose and throat surgeons, oral surgeons and plastic/reconstructive surgeons), medical oncologists, dentists, dieticians, speech pathologists, physiotherapists, occupational therapists, cancer nurses, psychologists, social workers and cancer care coordinators.
Radiation Therapy (also called radiotherapy) is often used as the primary treatment for cancers in the head and neck region. In particular, cancers of the throat are often treated with curative radiation therapy alone, especially if they are early stage cancers and surgery may involve loss of function.
This approach can allow the preservation of normal organ function such as speech, whilst maintaining acceptable cosmetic results. Chemotherapy may be used during radiation therapy treatment to enhance the cancer killing effect of radiation therapy.
In some cases, radiation therapy may be required in addition to surgery. Cancers that arise in the sinuses are treated primarily with surgery with or without radiation therapy and chemotherapy. Similarly, cancers arising the in salivary glands are typically treated with surgery alone with or without radiation therapy afterwards.
External beam radiation therapy is the most common type of radiation therapy used in head and neck cancers and requires a meticulous planning process. Intensity-modulated radiation therapy (IMRT) or volumetric arc therapy (VMAT) utilises advanced technology to precisely deliver the radiation to the specific areas that need to be treated. This reduces the dose of radiation reaching or damaging important structures such as the salivary glands in the head and neck region.
Radiation therapy is usually delivered once a day, five days a week from Monday to Friday and requires a multidisciplinary approach. It is important not to have any unplanned treatment interruptions to get the maximum benefit from treatment. Towards the end of a patient’s radiation therapy, some patients may receive two treatments a day to make up for any missed days. The total length of treatment time will vary from 5-7 weeks.
-
What are the Side Effects of Radiation Therapy?
The potential side effects from radiation therapy of the head and neck region can be divided in to early (during or immediately after treatment and usually temporary) or late (months after treatment and can be persistent).
Generally speaking, radiation therapy can cause tiredness, lethargy and skin reaction that usually settles within four to six weeks. Other, more specific side effects come from the structures/organs in and just next to where the radiation is being targeted and include throat or mouth pain, dry mouth, altered taste, thick mucous secretions, swallowing issues and dental problems.
Side effects may include, but are not limited to:
Early or ‘acute’ side effects (usually occur 1-2 weeks after starting treatment, persisting for a few weeks)
Fatigue is a common side effect of radiation therapy and is more likely to occur in the second half of treatment and is variable between patients. This may persist for a few weeks after treatment and usually settles within 4-6 weeks once radiation therapy is completed.
Redness, irritation and soreness in the mouth/throat causing pain and difficulty in swallowing – pain in the mouth and throat can occur a few weeks into radiation therapy relating to mucosal changes, including ulcer formation. This may have an impact on nutrition due to swallowing difficulty. Involvement of a dietitian will be important during the treatment course. Your treating team can advise you on pain killers and oral care including mouth washes that may assist in this area. In some cases, a feeding tube may be recommended. This problem can take 4-6 weeks following treatment to improve.
Dry mouth and/or thick saliva – the glands that produce oral saliva can be affected by radiation resulting in a dry mouth and thick secretions. A dry mouth can be either temporary or permanent. It will be important to keep the mouth moist by drinking water. Artificial saliva may also help. If you develop thick mucous secretions, salt water mouth washes can help this temporary problem.
Altered taste and/or loss of appetite– some patients report either loss of taste or altered taste e.g. sweet foods may taste salty or metallic. This can have an affect one’s ability to enjoy food and consequently affect appetite. This is usually a temporary problem but for some may be permanent.
Skin changes – redness, swelling and changes in the texture of the skin can occur. Some patients may notice some itching. This usually settles down within 4-6 weeks after treatment and can be relieved by creams on advice from the treating team. Sometimes, the skin can breakdown requiring dressings.
Hair loss – Hair loss can occur in the area that is being treated and at least some of it will be permanent.
Earache or blocked sensation of the ear can occur due to swelling of the eustachian tube (a tube that connects the middle ear to the back of the nose).
Hoarseness of voice – change in voice may occur if there is swelling and irritation of the voice box from the treatment.
Breathing Difficulty – the airway can become inflamed and swollen within the neck. In some rare cases, this swelling can be significant resulting in noisy breathing which requires a review by your treating team as soon as possible.
Late or long-term side effects (Side effects well after treatment)
Late side effects may occur a few months or years after treatment though they are much rarer than early side effects. Depending on the problem these may occur once and then go or may be more persistent over the long term or may come and go over time.
Likely side effects
Dry mouth – for some patients having a dry mouth may persist, although most centres employ a technique called IMRT to reduce the chance of this occurring. It will be important to keep the mouth moist by drinking water regularly and/or using an artificial saliva.
Underactivity of the thyroid gland – an underactive thyroid gland due to radiation therapy can make patients feel tired and lethargic. This can be determined by a blood test and if confirmed can usually be rectified by having thyroid medication prescribed by your doctor.
Neck stiffness – sometimes the soft tissues of the neck can become hard and stiff. This may have some impact on your neck range of movement and physiotherapy can help if this is the case.
Neck swelling – Some patients notice a swelling in the neck, commonly under the chin due to poor flow of lymph fluid. This is usually worse if your lymph glands have been removed at surgery. A physiotherapist or occupational therapist who specialises in lymphoedema management will help you to manage this. This may improve with time and is usually a cosmetic problem.
Swallowing complications – some patients may develop problems with swallowing after treatment such as difficulty and/or pain due to a combination of radiation therapy, surgery and/or the cancer itself. Your speech pathologist can assist with rehabilitation and recovery.
Hair loss – Permanent hair loss can occur in the area that has been treated.
Skin changes – thinning and dryness of skin, visible prominent blood vessels and change in skin pigmentation can occur years after treatment.
Teeth and jaw issues – the teeth are more at risk of developing tooth decay. It is important to maintain good oral hygiene and regular dental checks after treatment. Your dentist should always be made aware that you have had radiation therapy.
Change in voice – Hoarseness of voice usually recovers after treatment but in some cases, it may last for several months. Rarely, there may be permanent change in voice quality, especially when the voice box (larynx) is treated.
Rarely
Soft tissue damage causing chronic non healing ulcers (an open sore)
Damage to the jaw bone usually after post treatment dental surgery or other trauma. It occurs due to a limited ability to repair and an increased susceptibility to infections.
Breathing difficulty due to airway swelling (rarely requiring tracheotomy).
Narrowing of the arteries – there may be an increased risk of developing a stroke in the future if the arteries to the brain are affected by radiation therapy. To reduce the risk of this occurring, patients should address risk factors such as controlling blood pressure, regular exercise and stopping smoking.
Very rarely
Nerve/spinal cord injury – Irritation of the spinal cord causing an electric-like sensation with neck flexion can occur several months after treatment. This usually requires no treatment and resolves by itself. Any long term effects are very unlikely.
Cataract
Second cancer – Any exposure to radiation increases the risk of a second cancer developing in that area, usually several years later. This risk is not entirely attributable to radiation received as part of your treatment. All X-rays and scans received over your lifetime contribute to this risk, as does unavoidable exposure to environmental radiation. The risk of a cancer being caused by radiation therapy decreases with increasing age and is in the order of 0.5 – 1% at 10 years.
-
How Do I Enquire About Radiation Therapy with My Healthcare Professional?
The best person to discuss radiation therapy for head and neck cancer with is a Radiation Oncologist. Your general practitioner or surgeon can refer you to a radiation oncologist (specialist doctor) to discuss whether radiation therapy is appropriate for you.
Visit ‘For GPs and other Health Professionals’ and ‘Talking to your doctor’ sections for further information.
Find your closest radiation oncology Treatment Centre
Useful Resources:
Patient story – Lex was diagnosed with a 4cm cancerous tumour at the back of his tongue and began radiation therapy at a regional centre in Queensland. Watch the start of his inspiring story as he talks about the multi-disciplinary team supporting him and his family.
Head and Neck Cancer Patient Support Book produced by ‘The Swallows’ Head & Neck Cancer Support Group
Head and Neck Cancer Forum 2020 which includes a unique series of 14 videos on innovations in the treatment of head and neck cancer patients. Videos focused on radiation therapy look at technology innovations in radiation therapy and managing mask anxiety.
Visit Julie’s facebook page which contains encouraging & helpful information for Head & Neck Cancer patients, families, friends & clinicians https://m.facebook.com/headandneckcanceraustralia/
Page last updated: 16/12/2020




